Table of Contents
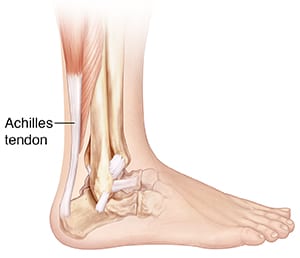
What is the Achilles Tendon?
The Achilles tendon is the band of tissue that runs down the back of the lower leg, connecting the calf muscle to the heel bone. Also known as the heel cord, the Achilles tendon facilitates walking by helping to raise the heel off the ground prior to the push-off phase of gait.
Achilles Tendinitis, Achilles Tendinosis, and Achilles Tendon Rupture
Two common disorders that occur in the heel cord are Achilles tendinitis and Achilles tendinosis. The third disorder, Achilles Tendon rupture, is rare and will be discussed in another article.
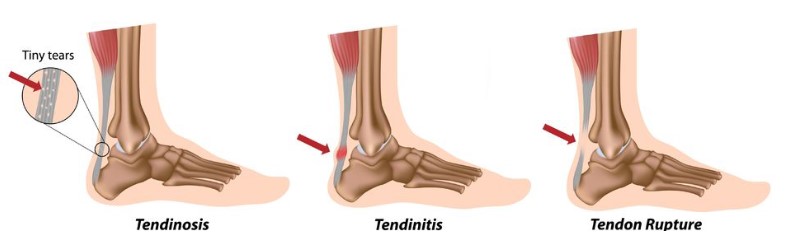
Achilles tendinitis is inflammation of the Achilles tendon. This inflammation is typically short-lived. Over time, if not resolved, the condition may progress to a degeneration of the tendon (Achilles tendinosis), in which the tendon loses its organized structure and is likely to develop microscopic tears and thickening. Sometimes the degeneration involves the site where the Achilles tendon attaches to the heel bone, other times it’s located in the middle of the tendon. In rare instances, patients can have Achilles tendinosis for a long period, with or without pain, which may result in an Achilles tendon rupture.
Causes
Achilles tendinitis and tendinosis are usually caused by a sudden increase or repetitive activity involving the Achilles tendon. Such activity puts too much stress on the tendon too quickly, leading to micro-injury of the tendon fibers. Due to this ongoing stress on the tendon, as well as overuse from certain activities such as sports, the body is unable to repair the injured tissue. The structure of the tendon is then altered, resulting in continued pain and swelling. What makes things worse is much of the Achilles tendon does not have a direct blood supply, so healing the damage is much more difficult.
Athletes are at a high risk for developing Achilles tendon disorders. Achilles tendinitis and tendinosis are also common in individuals whose work puts stress on their ankles and feet, such as manual laborers. With the increased number people out there doing activities such as CrossFit and high-intensity, explosive workouts, the numbers of Achilles injuries is increasing.
Additionally, people with excessively pronated or flattened feet have a tendency to develop Achilles tendinitis and tendinosis due to the greater demands placed on the tendon when walking. The Achilles tendon not only has a north-south stretch placed on it, it also has a twisting force as well. To an area with relatively little blood flow, this only makes things worse. If these individuals wear shoes without adequate stability, their overpronation could further aggravate the Achilles tendon.
Symptoms
The symptoms associated with Achilles tendinitis and tendinosis include:
- Pain: aching, firmness, soreness within the tendon. This may occur anywhere along the tendon’s length, beginning with the tendon’s attachment directly behind the heel upward to the area below the calf muscle. Pain often appears upon getting out of bed in the morning or standing after periods of rest, then improves somewhat with motion. In some cases, people report the opposite: it isn’t too painful upon first getting out of bed or after periods of rest, but as they increased motion or activity, it feels progressively worse.
- Tenderness, or sometimes sharp pain, when the sides of the tendon are squeezed.
- When the disorder progresses to degeneration, the tendon may become enlarged and may develop firm nodules in the area where the tissue is damaged.
Diagnosis
In diagnosing Achilles tendinitis or tendinosis, the doctor will examine your foot and ankle and evaluate the range of motion and condition of the tendon. The area can be further assessed with x-rays, sonography (ultrasound), or MRI (magnetic resonance imaging). It’s important to note that x-rays do not detail tendons very well, but the doctor would be interested in observing general swelling within and around the tendon, as well as bone and joint structures of the foot and ankle. Bone spurs of the heel can be seen in some cases.
Conservative Treatment
Treatment approaches for Achilles tendinitis or tendinosis are selected on the basis of how long the injury has been present and the degree of damage to the tendon. In the early stage, when there is sudden (acute) inflammation, one or more of the following options may be recommended:
- Immobilization. Immobilization may involve the use of a cast, posterior splint, or removable walking boot to reduce forces through the Achilles tendon and promote healing.
- Ice. To reduce swelling due to inflammation, apply a bag of ice over a thin towel to the affected area for 20 minutes of each waking hour. Do not put ice directly against the skin.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be helpful in reducing the pain and inflammation in the early stage of the condition.
- Orthotics. For those with overpronation or gait abnormalities, custom orthotic devices may be prescribed.
- Night splints. Night splints help to maintain a stretch in the Achilles tendon during sleep.
- Physical therapy. Physical therapy may include strengthening exercises, soft-tissue massage/mobilization, gait and running re-education, stretching and ultrasound therapy.
Surgery
Prevention
Achilles Tendon Disorders in Orange County
If you are suffering from an injury to the Achilles tendon, do not hesitate to call us or request an appointment online. Our doctors are well-versed in this condition and can develop an effective treatment course to get you back in action as soon as possible.